How do we create the continuum of care?
The dream of a unified health service, with the seamless exchange of information across healthcare systems and professionals, is no longer a distant dream. On the contrary. In fact, both the technology and digitalisation are in place. Rather, it is a question of deciding on a shared vision and approach.
Since the 1970s, Denmark has led the way within message-based information exchange in the health and social sector. The exchanges are based on one-way communication, where the sender decides what the recipient can read.
This has, among other things, resulted in effective solutions such as the Danish eHealth portal ‘Sundhedsjournalen’ (www.sundhed.dk), which is widely used today and gives citizens access to much of their health data.
Denmark’s leading position within information exchange has played a decisive role in our ability to build up an efficient, modern, and citizen-focused public sector.
“The existing communication is based on an approach where the sender decides what sort of information the recipient can access. It functions extremely well in many cases, but when a doctor, district nurse or medical specialist needs additional information about a patient’s treatment, for example observations or additional treatments, it’s not always possible,” says Mikkel Harbo, Director, Business Development & Product Management, at Systematic.
The approach can therefore lead to unfortunate situations and costly decisions that benefit neither the citizen nor society.
Simple access to real-time data
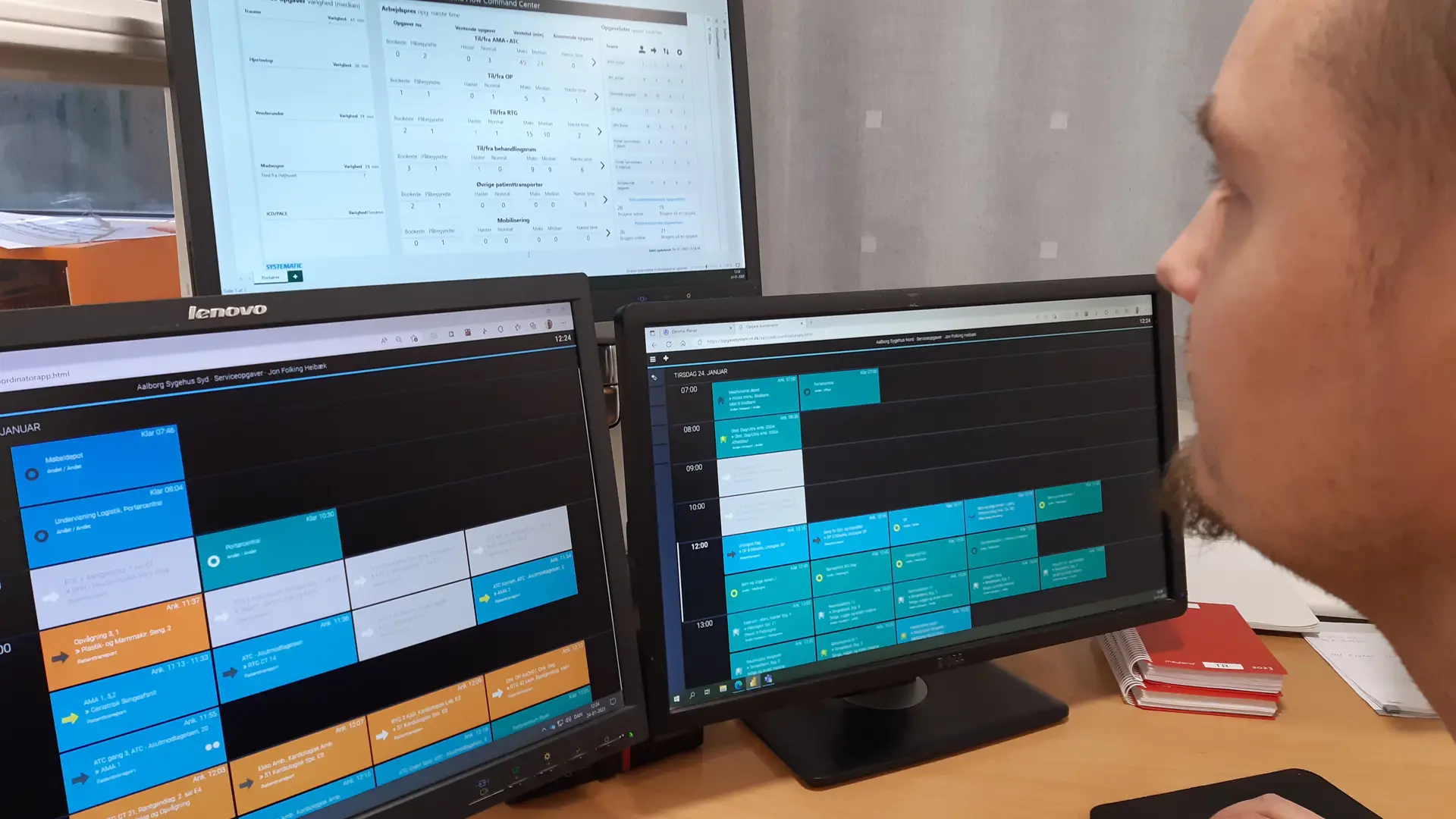
The solution is to create the continuum of care. The idea of a unified health service is based on a principle of simple access to real-time data and information, where social and healthcare professionals can easily access relevant data on citizens and patients which are crucial for a given assessment or treatment.

“The continuum of care requires a paradigm shift in relation to how information is currently exchanged. More user-friendly and simpler access to a citizen’s health data should in future be ensured by merging data from all health providers into the individual clinician’s system. By ensuring such simple access to information, we create greater coherence in a patient/citizen process, which not only supports more effective treatment and a better experience for the citizen, it also ensures faster case processing in the municipalities, increased quality and greater interaction between individuals and different professional groups,” says Mikkel Harbo and continues:
Citizen and patient-centric
The exchange of information between the hospital system, the municipal social and health services and private specialist doctors is vital for good and effective citizen-focused treatment.
If the needs of a patient or citizen develop significantly from the latest information registration, this may, at worst, result in inappropriate courses of treatment and costly extra expenses for society. Simply because the data which is required to make the best decisions is not available.
“If, for example, an older patient is discharged following hospital admission, and where they have been given medicine to take home, it may be unclear whether the medicine was given when the patient was discharged – or whether the home care services had to give it subsequently. This uncertainty may cause the home care services to contact the hospital, and if the patient does not receive the medicine, it might even result in them being readmitted. In other words, a less than desirable course of action for the patient, staff, and the hospital,” says Mikkel Harbo.
By bringing together hospital employees, doctors, municipal healthcare professionals and the citizen, the continuum of care ensures a better, cheaper and more efficient approach.
A new approach to treatment
Thus, there are obvious advantages in ensuring greater connectivity across the health services by facilitating access to more information, but this does not mean that it is necessarily simple to implement.
In Denmark, we operate according to a principle of ‘equal health for all’. A basic idea that ensures fair and effective treatment for all Danes – regardless of background. For this reason, it is difficult to introduce systems that will lead to better treatment and procedures for some citizens and professionals if they are not rolled out widely from the outset.
Isolated solutions will compromise a cornerstone of the Danish model and require a fundamental decision to accept differences in the treatment that individual citizens receive until the solutions can be rolled out nationally. This means that even though the digital solutions are in fact staring us in the eye, and Danish system suppliers can in principle already deploy a unified health service, it is not possible.
The individual IT systems that can ensure coherence and support treatment systems across the board already exist, and if they are implemented individually, the experience can eventually form the basis for national solutions and be incorporated in the overall system as they are established.
How do we achieve our objectives?
It is a question of creating a coherent ecosystem that grows and develops while spanning users, citizens, and suppliers – and which benefits society as a whole. On this basis, we can create solutions that meet the needs of the healthcare professionals at the hospital, in the municipality, at the care home and in citizens’ private homes.
“We have all the pieces we need to complete the jigsaw. Now, we have to find out how we fit them together through open, transparent systems that support all parts of the citizen’s health journey – and the daily work of the professionals. This requires open solutions that are geared for the future which suppliers can build on independently of who originally developed them,” says Mikkel Harbo.
Explore our vision of a complete continuum of care
At Systematic, we strive to enable the complete continuum of care across the entire healthcare provision chain and centred around the citizen. We aspire to bring together hospitals, doctors, municipal care providers and citizens to form one health journey.
Latest cases
Our solutions and services make a difference to our customers. Take a look at our cases and find inspiration in the benefits others have realised.