TL;DR (summary): A mix of published NHS pilots, independent evidence and sector reports shows that poor equipment visibility wastes clinician time, drives unnecessary purchasing, and increases compliance risk. Targeted, standards-based pilots (barcodes → RFID → RTLS) return measurable clinical time and inventory savings for NHS Trusts when implemented with clear guidelines, baseline metrics, and staff engagement. This long-read explains the evidence, practical deployment choices, ROI expectations, and the implementation checklist NHS Trusts need to reduce waste and free time for patient care.
Why equipment visibility matters now
Hospitals across the NHS manage billions of pounds worth of medical equipment. When items are misplaced or poorly tracked, the result is wasted time, wasted money, and delays in patient care. While some headline figures in the public conversation are overstated, reliable data from NHS pilots, government reports, peer-reviewed research, and recent deployments provide unmistakable evidence of the benefits of digital equipment tracking.
This guide focuses on five evidence-based insights that show how NHS Trusts can save money, reclaim staff time, and strengthen compliance with modern equipment tracking.
1. Equipment loss is a real and costly issue
NHS organisations spend significant sums replacing unreturned or misplaced kit. A 2019 Freedom of Information exercise reported by NHS England showed that 66 Trusts spent more than £14 million replacing an estimated 560,000 walking aids over five years. Walking aids are relatively low-cost items, yet the total ran into millions. The implication is clear: if this loss occurs with basic equipment, the impact across higher-value devices will likely be material.
The National Audit Office's 2024 report highlighted wide price variation and duplicated effort in NHS procurement. It was found that the NHS continues to spend more than £3 billion outside the NHS Supply Chain, its purpose-built procurement route, as customer satisfaction has declined. These issues extend into inventory management. Where visibility is weak, losses are often hidden in routine spend lines and do not trigger the controls they should.
2. Staff time lost searching for equipment
Time is the most valuable resource in healthcare. A peer-reviewed study in the Future Hospital Journal found that doctors spent about 13% of their time searching for equipment and paperwork. Across a Trust, this quickly adds up to many clinical hours.
Recent NHS pilots show what can be recovered. In 2024, as part of NHS England's Wireless Trials programme, Mid Cheshire Hospitals NHS Foundation Trust and Princess Alexandra Hospital NHS Trust received funding to install wireless trackers on medical equipment and hospital beds for real-time monitoring and location tracking.

Annual impact:
187 hours per year saved per clinician
Equivalent to nearly five additional weeks of patient care time annually
Across a typical Trust with 200 clinical staff: 37,400 hours recovered per year
The savings shown represent the average time recovered per individual clinician (doctor or nurse) each week. The estimates are based on a combination of direct time-motion observations and survey responses, as documented in peer-reviewed NHS studies. The aim is to help staff easily find what they need when they need it, ultimately freeing up more time for staff to spend with patients.
Every minute spent looking for a device is a minute not spent with a patient. Real-time visibility changes that equation.
3. Proven savings from NHS pilots
When Trusts can see where equipment is and how it moves, costs start to fall. The Scan4Safety programme across six demonstrator Trusts reported impressive results: 140,000 clinical hours released to care, £5 million in recurrent inventory savings, and £9 million in non-recurrent inventory reductions over the two-year programme period.
Individual Trust results were equally compelling. At University Hospitals of Derby and Burton NHS Foundation Trust, cumulative benefits of £3.2 million were realised by December 2018 following the introduction in April 2016. Leeds Teaching Hospitals NHS Trust reduced the average product recall time from 8.33 days to less than 35 minutes, resulting in estimated annual savings of £84,411 on recalls alone.
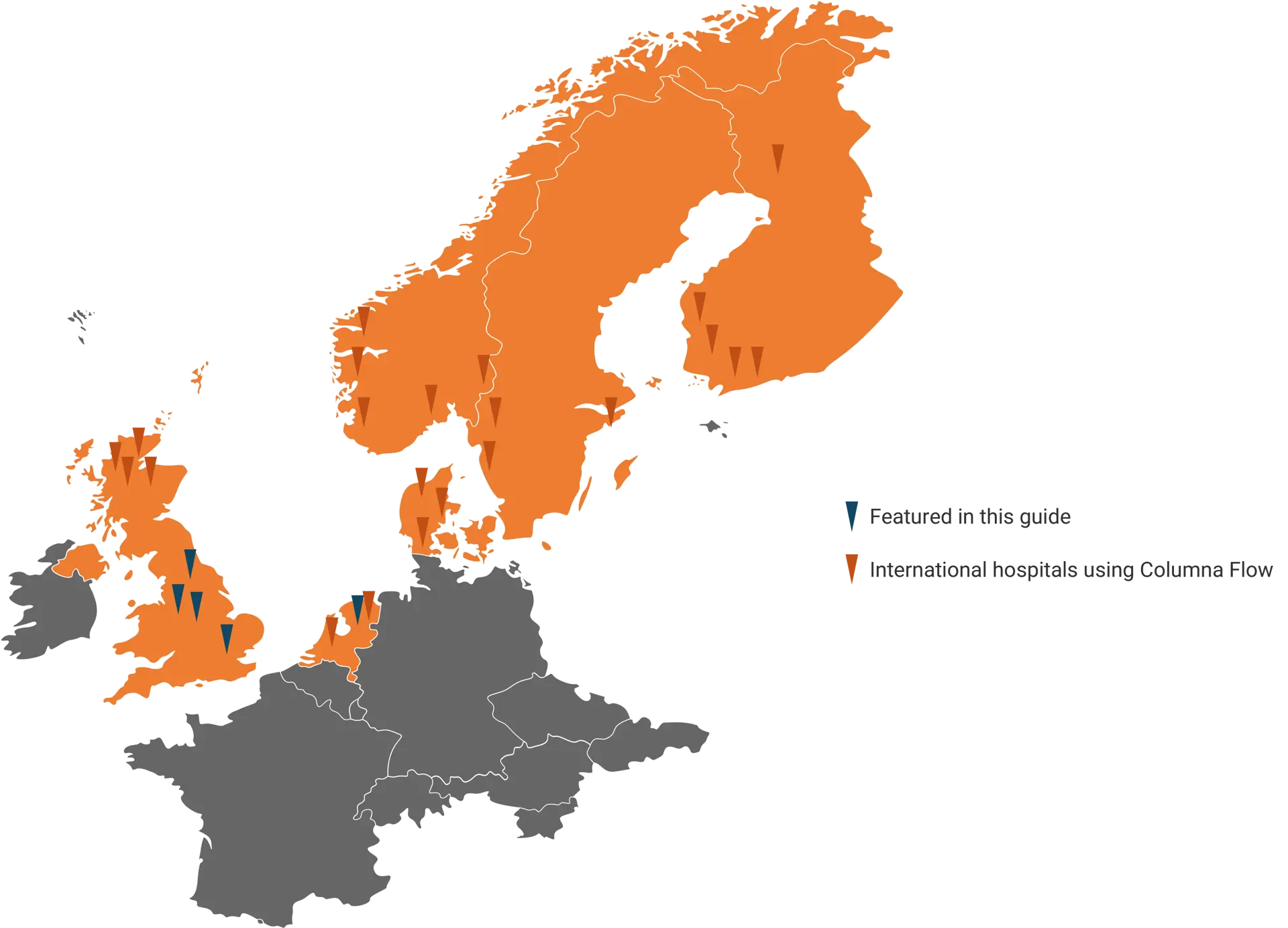
There is also fresh evidence of real-world deployments outside the UK. At the University Medical Centre Groningen in the Netherlands, Systematic's Search and Find platform is being implemented to locate equipment, beds, and personnel in real time through mobile devices. The hospital expects gains in faster location, optimised stock levels, and automated maintenance and cleaning workflows.
Unlock the benefits of equipment tracking and streamlined workflows at your hospital.
Hospitals across Europe already use Search & Find to cut wasted time and avoid unnecessary costs.
4. ROI and payback timelines
Procurement teams need to know when an investment will pay for itself. Evidence from NHS pilots points to rapid payback. The Scan4Safety evidence report documents substantial non-recurrent and recurrent savings within the two-year Scan4Safety programme period. Individual site results show strong returns: Derby Teaching Hospitals realised £3.2 million in cumulative benefits, while Leeds Teaching Hospitals reported £2.3 million in cumulative savings.
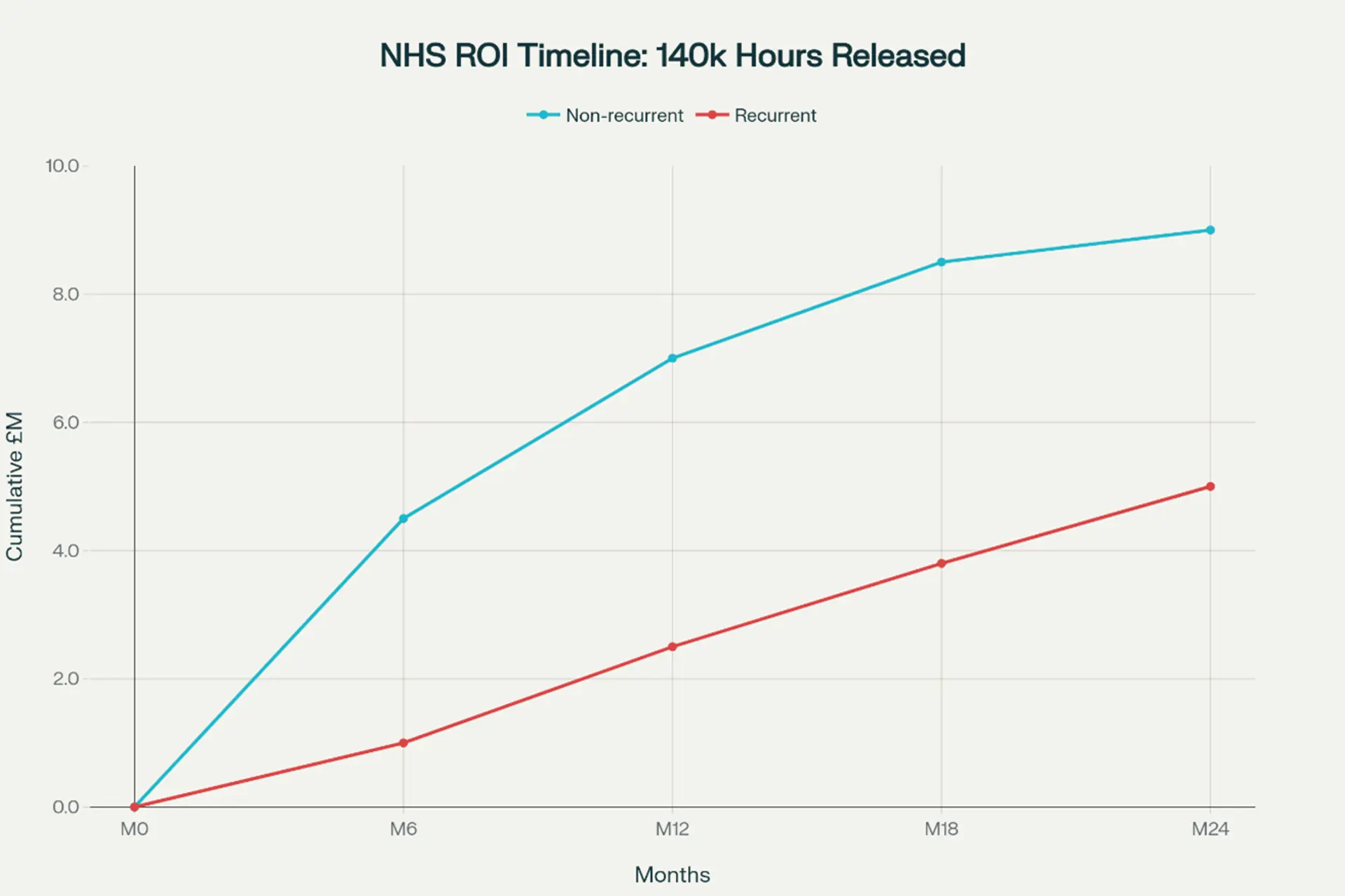
The visualisation demonstrates the typical two-year payback pattern that NHS Trusts can expect when implementing equipment tracking systems, based on the verified Scan4Safety evidence. For large trusts like Derby and Leeds, even modest savings can have a significant impact, freeing up resources from a billion-pound budget to support frontline care in line with NHS best practices.
⏱️ Timeline for implementation:
Months 0-6: Initial deployment and early inventory optimisation
Months 6-12: Systems bedding in, workflow improvements emerging
Months 12-18: Full deployment benefits realised
Months 18-24: Sustained operational efficiencies established
Trusts that phase deployments tend to see quicker returns. Start with high-value mobile assets, use existing Wi-Fi infrastructure, and expand as the data shows what to optimise next. The financial case strengthens as duplicate orders decrease, rentals decline, preventive maintenance is scheduled on time, and clinical space is utilised more effectively.
See what ROI could look like in your own Trust. Our team can tailor a demo based on your environment and priorities.
5. Patient safety and compliance benefits
The case for tracking is not just financial. In urgent scenarios, delays in locating equipment can affect outcomes. Systems that make device location and status visible reduce delays and increase confidence that the right equipment is where it is needed.
Regulation supports this approach. The Care Quality Commission requires equipment to be suitable, maintained, and stored securely under Regulation 15: Premises and Equipment. The Medicines and Healthcare Products Regulatory Agency sets expectations for systematic medical device management, including accurate device usage records, maintenance, and incident reporting. Real-time visibility makes compliance simpler by building evidence into daily workflows.

Recent European deployments show how the same principles apply outside the UK. UMCG's Search and Find rollout is designed to ensure that critical devices are available and clean when needed, with automated triggers for maintenance and cleaning that reduce risk and support patient safety.
Technology choices for NHS Trusts
Choosing the right technology starts with building a strong business case. The critical questions are what level of tracking precision is required and what the licence and maintenance costs will be. Today's options include barcodes, RFID, BLE, Wi-Fi, ultrasound, and infrared.
Customers often ask: Which one should we use?
The answer depends on your use case. Start with the outcomes and workflows you need to achieve, then match the technology to the problem.
Barcodes are a low-cost and effective solution for basic inventory control, although they require line-of-sight scanning. RFID drives low maintenance costs and works across almost every equipment type. BLE solutions, such as Wirepas, are easy to install and scale in existing buildings. IoT and real-time location systems provide continuous monitoring across large estates and can integrate with existing systems.
Most Trusts will benefit from a hybrid approach. A practical way to begin is with a lightweight pilot, giving end users real products they can test and work with. This hands-on approach validates assumptions, refines workflows, and ensures the chosen technology delivers measurable value before wider deployment.
Learn more about our low cost BLE Tracking solution - Tracklite.
Deployment readiness checklist
Business case and outcomes
Have you defined the overall business outcome you're working towards?
Which specific use cases will support that outcome?
Have clinical, estates, and procurement teams agreed on target assets and baseline metrics?
Technology and integration
What tracking technology best supports your use cases?
Is the existing Wi-Fi and network coverage reliable when assets are in motion and stored?
How will the system integrate with current digital systems, such as Electronic Health Records (EHR), Computerised Maintenance Management System (CMMS), asset management, and logistical workflow solutions?
Are GS1 standards part of the plan, including device and location identifiers?
People and workflows
Which end-user roles are targeted, and how should they be involved?
Who should have ownership of the solution?
How should the use cases be integrated into existing workflows and applications?
What training and change support do ward teams, porters, and technical teams need for the first pilot?
Conclusion
The combined evidence from FOI investigations, national audit work, case studies, peer-reviewed studies, and NHS pilots indicates that equipment loss and wasted searching persist as significant problems.
Digital tracking reduces waste, returns time to care, and simplifies compliance. NHS Trusts that start with clear objectives, phased deployments, and measure results unlock the most outstanding value for patients and staff.
Equipment tracking FAQs
There is no single national figure. Verified FOI data shows £14 million on replacement walking aids over five years by 66 Trusts. Pilots and audit reports evidence broader losses.
A peer-reviewed study found about 13% of working time spent searching for equipment and paperwork. NHS pilots confirm measurable time savings once tracking is introduced.
Scan4Safety evidence and several case studies indicate substantial savings within two years, with some Trusts reporting multi-million pound cumulative benefits.
Barcodes, RFID (Radio Frequency Identification), and IoT (Internet of Things) or RTLS (Real Time Location System) are often used together. Alternatives such as Bluetooth, infrared, ultrasound, and wi-fi are also viable. Choose based on workflow needs and asset criticality.
Beyond just software or hardware, the future vision is to offer NHS Trusts a complete solution package through trusted partnerships. This means preferred vendors collaborate to deliver tailored combinations of technology, integration, training, and support - creating an end-to-end service unique to each Trust’s needs. This approach simplifies deployment, accelerates benefits, and ensures a seamless experience, much like the comprehensive solutions that Systematic is pioneering.
References
1. NHS England North West (2019). NHS spent over £14 million on replacement walking aids over five years. Available: https://www.england.nhs.uk/north-west/greener-nhs/case-studies-greener-nhs/case-study-walking-aids/. Accessed 26 August 2025.
2. National Audit Office (2024). NHS Supply Chain and efficiencies in procurement. Available: https://www.nao.org.uk/reports/nhs-supply-chain-and-efficiencies-in-procurement/. Accessed 26 August 2025.
3. Milne, R. et al. (2016). How much of a doctor's on call shift is spent searching for equipment and paperwork. Future Hospital Journal, 3(3), 164-167. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6465898/. Accessed 26 August 2025.
4. NHS England (2024). £1 million boost for wireless innovations to improve patient care. Available: https://www.england.nhs.uk/2024/02/1-million-boost-for-wireless-innovations-to-improve-patient-care/. Accessed 26 August 2025.
5. GS1 UK (2018). A scan of the benefits: the Scan4Safety evidence report. Available: https://scan4safety.nhs.uk/evidence/. Accessed 26 August 2025.
6. Care Quality Commission. Regulation 15: Premises and Equipment. Available: https://www.cqc.org.uk/guidance-providers/regulations-enforcement/regulation-15-premises-equipment. Accessed 26 August 2025.
7. Medicines and Healthcare products Regulatory Agency (2021). Managing Medical Devices guidance. Available: https://assets.publishing.service.gov.uk/media/6089dc938fa8f51b91f3d82f/Managing_medical_devices.pdf. Accessed 26 August 2025.
8. Systematic (2024). Smart digital solution enhances medical equipment utilisation and saves costs. Available: https://systematic.com/int/industries/healthcare/news/news/flow-search-find-in-groningen/. Accessed 26 August 2025.
Latest cases
Our solutions and services make a difference to our customers. Take a look at our cases and find inspiration in the benefits others have realised.